Welcome to My Blog! 🌟
I’m so glad you’re here! Before we jump into the exciting content, I’d love for you to connect with me on my social media platforms. It’s where I share extra insights, interact with our amazing community, and post regular updates. Here’s how you can join the conversation:
📘 Facebook: Follow me on Facebook for more updates
Now, let’s dive into the journey ahead. I hope you find everything here both engaging and valuable. Together, let’s explore, learn, and grow! 🚀
Table of Contents
Introduction
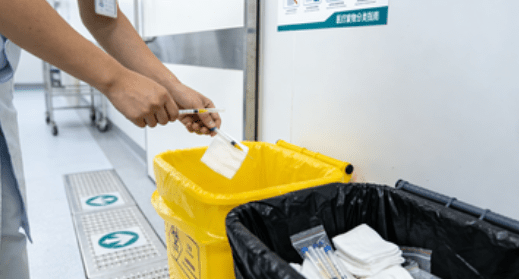
A medical incinerator is a specialized device used for the disposal of biomedical and clinical waste through high-temperature burning. This type of waste includes items contaminated with bodily fluids, sharp instruments, pharmaceutical residues, and pathological materials. Medical facilities, laboratories, and research institutions rely on this equipment to ensure a safe and hygienic environment for both workers and patients.
Unfortunately, many misconceptions surround the topic of medical incinerators. These myths often stem from outdated technologies, lack of understanding, or misinformation. As a result, they can discourage healthcare providers from implementing this effective waste disposal method.
In this blog, we will explore five widespread myths about medical incinerators, explain the truth behind them, and help you better understand why this equipment remains a crucial part of modern healthcare waste management.
Myth 1: A Medical Incinerator Is Harmful to the Environment
One of the most common misconceptions is that a medical incinerator causes environmental damage due to the emission of harmful gases and pollutants. While older models may have had issues with emissions, modern designs are built with advanced filtration systems and emission controls.
Understanding the Truth
Today’s medical incinerators are engineered with compliance in mind. Many models come equipped with scrubbers, secondary chambers, and particulate filters that significantly reduce the release of toxins such as dioxins and furans. Moreover, many countries enforce strict regulations on emissions, pushing manufacturers to develop cleaner and more efficient solutions.
Environmental Impact Table
Here’s a comparative overview of older versus modern medical incinerator systems:
| Feature | Old Medical Incinerators | Modern Medical Incinerators |
|---|---|---|
| Emissions Control | Limited or none | Advanced filtration systems |
| Fuel Efficiency | Low | High with automatic adjustments |
| Regulatory Compliance | Often non-compliant | Designed to meet international standards |
| Waste Residue | Higher volume of ash | Lower residue, easier disposal |
| Odor Management | Poor | Sealed chambers and odor control systems |
As shown, modern solutions address many of the concerns associated with outdated incinerators, offering a far safer and environmentally friendly approach.
Myth 2: Medical Incinerators Are Outdated and Replaced by Other Technologies
With the emergence of newer waste treatment options such as autoclaves, microwave disinfection units, and chemical neutralization systems, many have come to assume that the medical incinerator has become obsolete. This perception, however, is not only inaccurate—it also overlooks the essential role incineration continues to play in global healthcare waste management.
Why Incineration Remains Essential
While alternative technologies have their place, they are not universal solutions. Some medical waste types—such as cytotoxic pharmaceuticals, pathological specimens, certain chemicals, and highly infectious materials—require treatment at extremely high temperatures to ensure complete destruction. The medical incinerator remains the only practical and approved solution in many countries for managing these hazardous materials safely.
Unlike autoclaves, which can only sterilize waste, a medical incinerator reduces both the volume and toxicity of the material, turning dangerous substances into inert ash. This is especially crucial in handling items like contaminated sharps or tissues, which, if improperly treated, can transmit infections or pollute the environment.
Additionally, many national and international regulations still specify incineration as the primary or only acceptable treatment method for specific types of clinical waste. In developing regions or during emergency health responses, a medical incinerator often remains the most reliable, standalone solution. Its ability to operate independently of complex infrastructure makes it invaluable where resources are limited.
Myth 3: Operating a Medical Incinerator Is Too Expensive

Concerns about high energy consumption, maintenance fees, and labor costs have contributed to the myth that a medical incinerator is economically unfeasible for many healthcare institutions, especially smaller ones. While these concerns may have been more valid in the past, modern advancements have significantly changed the operational economics of these systems.
Breaking Down the Costs
Today’s medical incinerators are equipped with technologies that maximize efficiency and minimize fuel usage. Many systems include automatic ignition and shutdown controls, programmable cycles for different types of waste, and dual-chamber designs that optimize combustion. These innovations help cut fuel consumption dramatically compared to older models.
Maintenance has also improved. Components are now more durable and modular, allowing for easy servicing and longer operational life. By reducing dependence on third-party disposal contractors or frequent chemical treatments, a medical incinerator offers predictable and manageable costs over time.
Moreover, having on-site waste treatment capabilities allows healthcare facilities to streamline operations and reduce potential penalties or delays related to non-compliance. While the upfront investment may be substantial, the long-term savings—both in monetary terms and in improved safety and compliance—make the medical incinerator a financially sound decision for many organizations.
Myth 4: Medical Incinerators Are Not Safe to Operate
A persistent myth suggests that using a medical incinerator poses health and safety risks to staff, patients, and the surrounding community. This concern is largely based on outdated equipment that lacked sufficient safety controls. Today’s reality tells a much different story.
Modern Safety Features
Contemporary medical incinerators are built with strict safety standards in mind. Units commonly include sealed combustion chambers to prevent the release of harmful gases, emergency shutoff switches for immediate system halt, and automatic loading systems to minimize human contact with hazardous materials.
Many systems also come with remote monitoring and digital control panels, allowing operators to manage the machine without direct exposure. Temperature sensors and real-time alerts provide continuous oversight to ensure safe combustion and prevent operational errors.
Training and certification programs further enhance safety by equipping staff with the knowledge required to operate the equipment efficiently and responsibly. When paired with proper ventilation and emission controls, a modern medical incinerator poses minimal risk to users or the environment.
The combination of engineering advancements and institutional best practices has transformed the medical incinerator into one of the safest and most reliable waste treatment methods available to healthcare providers.
Myth 5: Medical Incinerators Can’t Be Used in Small or Remote Facilities

Some believe that only large hospitals or urban clinics can afford or accommodate a medical incinerator. This myth overlooks the diversity of incinerator sizes and configurations available today.
Scalable Solutions for Every Need
Manufacturers now offer a wide range of medical incinerators, including compact models suitable for small clinics, mobile units for field hospitals, and modular systems for scalable use. These options make it possible for rural and remote locations to benefit from safe waste disposal without depending on distant centralized facilities.
Medical incinerators are also crucial during health emergencies or in developing countries where waste management infrastructure is inadequate. Portable and diesel-powered units, for example, can provide a practical and immediate solution.
Conclusion
Dispelling myths about the medical incinerator is key to improving healthcare waste management. Far from being outdated, these modern, environmentally friendly machines play a vital role in safely disposing of hazardous materials, reducing disease risk, and ensuring regulatory compliance. With scalable, advanced designs, they offer long-term, effective solutions for facilities of all sizes. Understanding their real value helps healthcare providers make informed, sustainable decisions.
FAQ
What kind of waste can a medical incinerator handle?
A medical incinerator is capable of handling a variety of healthcare waste types, including sharps, human tissues, pharmaceuticals, soiled dressings, and other infectious or hazardous materials.
How do I ensure my facility meets emissions standards?
To comply with local and international emissions standards, it’s essential to invest in a certified model, perform regular maintenance, and monitor emissions using built-in diagnostics or third-party testing services.
Can small clinics afford to own a medical incinerator?
Yes, many manufacturers offer affordable, small-capacity models designed specifically for clinics, dental offices, and rural healthcare centers.
Do medical incinerators require a lot of maintenance?
Routine maintenance is required, but modern systems are built for durability and ease of use. Many units offer self-cleaning functions or require minimal manual intervention.
How long does it take to incinerate a batch of waste?
The time varies depending on the type and quantity of waste. On average, a standard batch may take 30 minutes to 2 hours, including cooldown and ash removal.