Table of Contents
Introduction

In the modern era of healthcare, managing infectious and hazardous medical waste is one of the most critical challenges facing hospitals, laboratories, and clinics worldwide. With increasing volumes of clinical waste generated daily from patient care, surgical procedures, pharmaceutical manufacturing, and laboratory research, safe and effective disposal has become essential for protecting both public health and the environment.
A Medical Waste Incinerator is not merely a disposal unit—it is a high‑temperature thermal oxidation system engineered to completely destroy infectious agents, chemical residues, and pharmaceutical contaminants. Operating typically between 850℃ and 1200℃, these systems ensure thermochemical oxidation of organic waste into harmless byproducts such as carbon dioxide, water vapor, and sterile ash, significantly reducing volume and sterilizing the waste stream.
However, the safe operation of a Medical Waste Incinerator involves far more than simply burning waste. It requires a meticulous approach to combustion control, waste preparation, emissions monitoring, operator training, and adherence to environmental standards set by regulatory authorities such as the U.S. Environmental Protection Agency (EPA) and national technical specifications like those from the Ministry of Ecology and Environment of China (HJ 177‑2023).
This comprehensive guide explores seven proven practices essential for optimizing Medical Waste Incinerator performance, improving safety, ensuring regulatory compliance, and maximizing operational productivity across healthcare and associated sectors.
Practice 1: Maintain Optimal High‑Temperature Combustion Parameters
Why Combustion Temperature Is Critical
The most fundamental principle in Medical Waste Incinerator operation is maintaining a stable, high‑temperature combustion environment. Research and regulatory guidelines indicate that effective sterilization and decomposition of biological and chemical hazards require sustained high temperatures—typically between 850℃ and 1200℃.
At these temperatures, the incinerator achieves complete oxidation, ensuring that all organic waste components are decomposed and that pathogens such as bacteria, viruses, and spores are effectively neutralized. Inefficient combustion can lead to incomplete oxidation, producing harmful emissions, toxic byproducts like dioxins and furans, and residual infectious material in the ash.
Advanced Temperature Monitoring and Control
Modern Medical Waste Incinerators incorporate digital temperature sensors, programmable logic controllers (PLCs), and feedback‑controlled fuel and air systems to maintain steady combustion. Operators should ensure that both primary and secondary chambers reach and sustain optimal temperature setpoints throughout the incineration cycle.
Best practices include:
- Continuous monitoring of combustion chamber temperatures
- Automated air/fuel adjustments based on real‑time data
- Calibration of sensors according to manufacturer schedules
- Maintaining residence times sufficient to complete oxidation
According to international technical advice, the use of secondary combustion chambers and controlled residence time (commonly 2 seconds or more) enhances complete destruction of hazardous components.
Impact on Pathogen Neutralization and Material Breakdown
Proper high‑temperature management directly affects the incinerator’s ability to neutralize biological hazards. Sustained temperatures above 1000℃ ensure that even heat‑resistant spores and complex chemical structures are fully decomposed into safer compounds, making this practice paramount for healthcare facilities.
Practice 2: Segregate, Classify, and Prepare Waste Correctly
Why Waste Segregation Matters
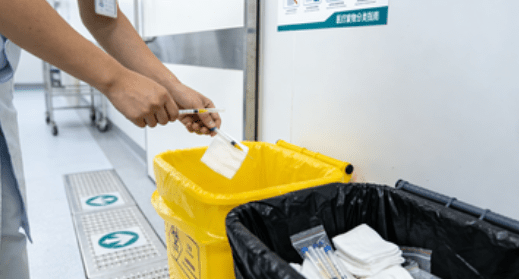
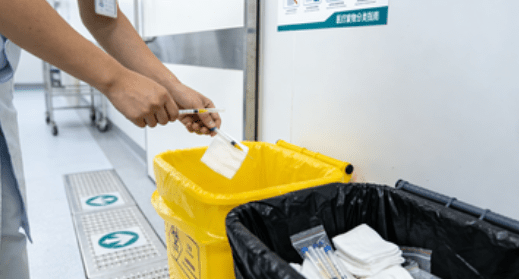
Before waste ever enters a Medical Waste Incinerator, it must be properly sorted to prevent hazardous combinations, optimize combustion, and comply with health regulations. Proper segregation helps reduce the risk of contamination, prevents dangerous reactions inside the incinerator, and improves overall combustion performance.
According to global medical waste management analyses, incorrect waste sorting is one of the leading causes of incinerator inefficiencies and increased operational costs.
Key segregation practices include:
- Separating infectious, chemical, pharmaceutical, and sharps waste
- Using designated containers with color‑coded identification
- Avoiding mixing high‑moisture waste or heavy metals with incinerable waste
- Labeling and securing hazardous waste bags to prevent leaks
How Segregation Enhances Combustion Efficiency
By sending only suitable materials into the Medical Waste Incinerator, operators can:
- Maintain stable combustion temperatures
- Reduce formation of toxic flue gases caused by inappropriate materials
- Improve thermal efficiency and reduce fuel consumption
- Lower the burden on emission control systems
Proper pre‑incineration waste management is not just efficient—it is crucial for preventing unintended release of pollutants and ensuring long‑term system stability.
Practice 3: Schedule Rigorous Routine Maintenance and Inspection
The Importance of Regular Maintenance
A Medical Waste Incinerator is a complex system with mechanical, electrical, and thermal components that must function harmoniously. Routine inspection and maintenance help prevent unexpected failures, reduce downtime, and extend the lifespan of critical parts such as burners, refractory linings, and emission control systems.
Core Maintenance Activities
Daily Tasks:
- Visual inspection of combustion chambers
- Checking fuel and air supply lines
- Verifying sensor readings and alarm systems
Weekly and Monthly Tasks:
- Removing ash and other residues from combustion chambers
- Inspecting refractory lining for cracks
- Cleaning or replacing air filters and exhaust ducts
Annual Inspection:
- Professional evaluation of the entire system
- Calibration of monitoring instruments
- Structural assessment of chambers and safety valves
By following a rigorous maintenance schedule, healthcare facilities can reduce the risk of system failures that might lead to incomplete incineration or regulatory non‑compliance.
Practice 4: Integrate Advanced Real‑Time Monitoring Systems
Why Monitoring Systems Are Essential
Real‑time monitoring technologies provide critical insights into combustion efficiency, emission quality, and system health. These systems collect data on chamber temperatures, oxygen levels, fuel consumption, and exhaust composition, enabling operators to make timely adjustments and prevent operational issues before they escalate.
Core Monitoring Components
- Digital temperature sensors in primary and secondary chambers
- Oxygen and carbon dioxide level detectors
- Emission analyzers for particulate matter (PM), nitrogen oxides (NOx), and other pollutants
- Automated alarms for critical threshold breaches
Benefits of Real‑Time Monitoring
- Early detection of incomplete combustion
- Lower fuel costs through optimized air/fuel ratios
- Enhanced compliance with regulatory standards
- Reduced risk of toxic emissions and environmental violations
Monitoring systems effectively act as the brain of modern Medical Waste Incinerator operations, increasing safety and performance while reducing costs.
Practice 5: Optimize Residence Time for Complete Oxidation

What Is Residence Time?
Residence time refers to the duration that waste and combustion products remain in the incinerator’s high‑temperature zone. Ensuring adequate residence time is essential for complete destruction of pathogens, organic toxins, and complex compounds.
Best Practices for Managing Residence Time
- Adjust residence time based on waste type (e.g., high‑moisture content requires longer time)
- Avoid overloading the incinerator to maintain uniform temperatures
- Use secondary combustion chambers to extend effective processing duration
- Coordinate with automated monitoring systems to optimize burn cycles
Properly managing residence time ensures deep oxidation, reduces the formation of hazardous byproducts, and enhances the overall efficiency of the Medical Waste Incinerator.
Medical Waste Incinerator Key Parameters and Performance Indicators
Below is a table summarizing key specifications, performance criteria, and operational benefits associated with efficient Medical Waste Incinerator practices:
| Parameter | Description | Operational Benefit |
|---|---|---|
| Combustion Temperature | 850℃–1200℃ | Ensures complete pathogen destruction |
| Residence Time | Adjustable per waste stream | Thorough oxidation, fewer residual toxins |
| Waste Volume Reduction | Up to ≥90% | Lower disposal costs, less landfill burden |
| Emission Controls | Filters, scrubbers | Reduced air pollutants and compliance with standards |
| Monitoring Systems | Real‑time sensors | Immediate adjustment, improved efficiency |
| Safety Protocols | Operator training | Reduced accidents, improved performance |
Practice 6: Train Operators and Implement Comprehensive Safety Protocols
Importance of Professional Training
A trained operator is one of the most critical factors in safe Medical Waste Incinerator operation. Without proper understanding of combustion dynamics, emission controls, and emergency procedures, even the most advanced system can perform poorly or pose safety risks.
Regulatory bodies such as the EPA emphasize comprehensive operator training to ensure compliance with emission standards and proper emergency handling.
Key Training Components
- Understanding combustion principles
- Waste classification and segregation techniques
- Emergency shutdown procedures
- Hazardous exposure prevention
- Emission control system operations
By ensuring that all operators receive documented training—and refresher training regularly—facilities can significantly reduce risks associated with incomplete combustion, equipment failure, or hazardous emissions.
Practice 7: Integrate Advanced Emission Control and Compliance Measures

Environmental Standards and Emission Targets
Incineration facilities that dispose of medical waste are subject to stringent emission standards to protect air quality. For example, regulations such as the EPA’s Hospital Medical Infectious Waste Incinerator standards limit pollutants including mercury, lead, cadmium, sulfur dioxide, and particulate matter.
International guidelines and national technical specifications (such as HJ 177‑2023 in China) require continuous monitoring, reporting, and odor control measures to minimize environmental impact.
Advanced Emission Control Technologies
- Multi‑stage scrubbers and filters
- Catalytic oxidizers to reduce volatile organic compounds
- Particulate matter capture systems
- Continuous emissions monitoring systems
These technologies help ensure that the Medical Waste Incinerator meets or exceeds air quality standards and protects community health.
Conclusion
Operating an effective Medical Waste Incinerator requires an integrated approach that combines advanced technology, skilled personnel, data‑driven monitoring, and strict adherence to regulatory standards. By implementing the seven proven practices outlined above—ranging from combustion control and waste segregation to operator training and emissions compliance—healthcare facilities can enhance productivity, reduce environmental impact, and safeguard public health.
Modern incineration technologies today not only neutralize biological hazards but also reduce waste volume by more than 90%, turning hazardous materials into manageable ash. As global healthcare systems continue to grow and medical waste generation increases, the adoption of robust Medical Waste Incinerator practices will remain essential for responsible waste management and sustainable operations.
FAQ
Q1: What types of waste should be incinerated?
Medical waste suitable for incineration includes infectious materials, pharmaceutical waste, sharps, and materials contaminated with biological agents, as outlined by regulatory and facility guidelines.
Q2: How often should a Medical Waste Incinerator be inspected?
Operators should conduct daily visual checks, weekly cleaning, monthly system calibrations, and annual structural assessments to maintain performance.
Q3: Are there environmental concerns with incineration?
With advanced emission control systems and adherence to regulatory standards, a Medical Waste Incinerator can meet international emission targets, significantly reducing harmful pollutants.
Q4: Can alternative technologies replace Medical Waste Incinerators?
Alternative treatments such as autoclaving or microwave processing exist, but they may not fully neutralize all hazardous waste streams, making incineration essential in many cases.
Q5: What role does monitoring play in incinerator management?
Real‑time monitoring allows immediate adjustments to combustion parameters and emissions, improving safety, efficiency, and regulatory compliance.